This research cluster focuses on basic and clinical aspects of deformity correction, bone biology, pathophyisiology and regeneration.
Deformity correction is the surgical adjustment or modification of bone that grows incorrectly due to a disease or occurs after a trauma. A limb deformity is characterized by any unnatural form, distortion or irregularity of an arm or leg.
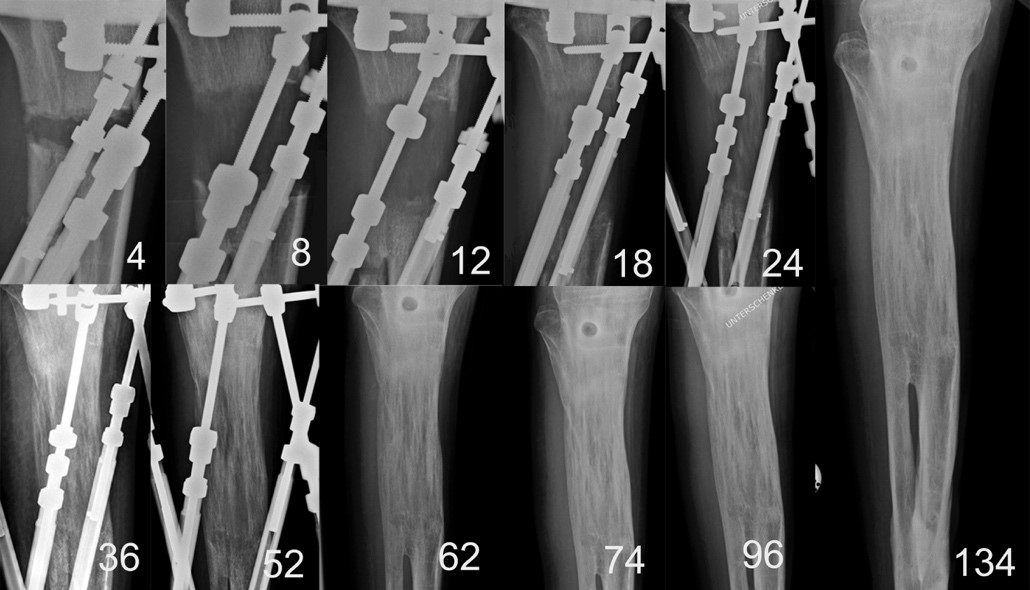
After a severe trauma, primary surgeries may be necessary to restore shaft fractures, joint fractures, bone loss, and the surrounding soft tissue with external fixators during Damage Control Orthopaedics (DCO) or with internal devices. If these procedures fail, secondary interventions can reconstruct limb length discrepancy, deformity, axial deviations, and impaired joint motion.
Limb deformities in growing child are caused by various things. Congenital deformities are those present at birth. Other limb deformities can occur later in life as a result of fracture, infection, arthritis or tumor.
These conditions are not just painful, they can severely impact lifestyle and mobility.
Reconstructive orthopedic and trauma surgeons may perform various operations to treat pain and functional issues. As axial deviations or misaligned bones can be corrected acutely, limb length discrepancy needs slow, gradual lengthening in an external frame or with an intramedullary telescopic nail.
Not only bone healing in deformity correction, but also fracture healing is a unique repair process in which the events of bone formation follow a specific time sequence. However, there are many ways in which these courses can be disrupted. Unsuccessful fracture healing as non-union is an orthopaedic and traumatologic condition with a high morbidity and clinical burden.
Principal investigators
- Ao.Univ.Prof. Dr. Catharina Chiari
ORCiD ID: 0000-0001-6275-7453
catharina.chiari@meduniwien.ac.at - Dr. Kolb Alexander
- Priv.Doz. Dr. Dr. Thomas Tiefenböck, MSc
ORCiD ID: 0000-0002-8698-8341
thomas.tiefenboeck@meduniwien.ac.at - PD Dr. Thomas Haider
- Dr. Gilbert Schwarz
- Dr. Rita Babeluk
- Dr. Greiner Fabian
- Dr. Kleiner Anne
- Priv.Doz. Dr. Lukas Zak
ORCiD ID: 0000-0002-1747-227X
lukas.zak@meduniwien.ac.at
Important publications
- Computed Tomography in Limb Salvage and Deformity Correction-3D Assessment, Indications, Radiation Exposure, and Safety Considerations.
Zak L, Tiefenboeck TM, Wozasek GE.J Clin Med. 2021 Aug 24;10(17):3781. doi: 10.3390/jcm10173781.PMID: 34501227 - The influence of advanced age in bone healing after intramedullary limb lengthening.
Zak L, Arnhold R, Tiefenboeck TM, Wozasek GE. Orthop Traumatol Surg Res. 2021 Sep 15:103055. doi: 10.1016/j.otsr.2021.103055. Online ahead of print. PMID: 34536594 - Bone reconstruction: subjective evaluation and objective analysis based on conventional digital x-rays - a retrospective evaluation.
Zak L, Tiefenboeck TM, Wozasek GE. Orthop Traumatol Surg Res. 2021 Sep 25:103081. doi: 10.1016/j.otsr.2021.103081. Online ahead of print. PMID: 34583012 - Intramedullary Bone Lengthening Following Preceding Hip Surgery-A Case Series.;
Zak L, Tiefenboeck TM, Wozasek GE. J Clin Med. 2020 Dec 19;9(12):E4104. doi: 10.3390/jcm9124104.PMID: 33352720 - Implant failure after externally magnetic-controlled nail lengthening.
Rentenberger C, Haider T, Zak L, Wozasek GE.Injury. 2021 Sep 9:S0020-1383(21)00758-0. doi: 10.1016/j.injury.2021.09.006. Online ahead of print.PMID: 34526237 - Anatomical Considerations of Intramedullary Humeral Nailing and Lengthening
Schwarz GM, Zak L, Hirtler L, Wozasek GE. J Clin Med. 2020 Mar 16;9(3):806. doi: 10.3390/jcm9030806.PMID: 32188086